Understanding Metabolic Syndrome and its Link to Diabetes
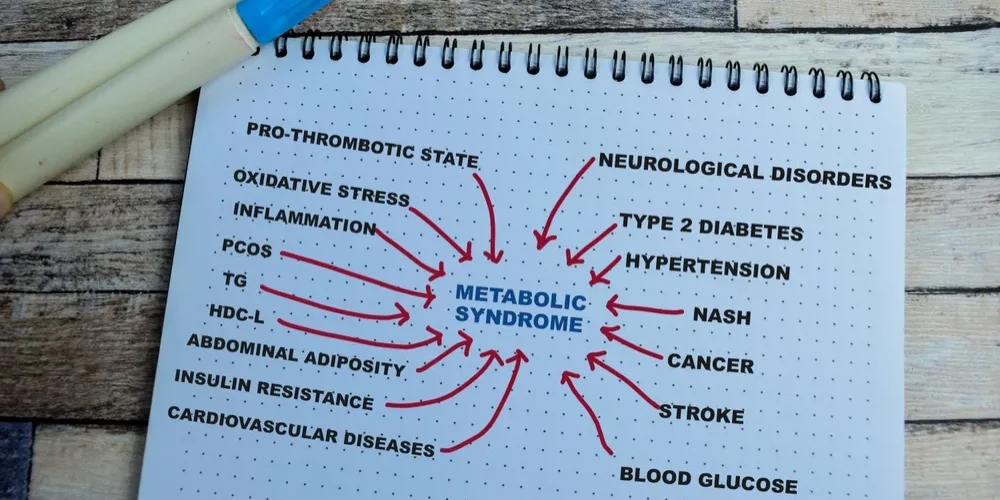
Metabolic syndrome, a sinister cluster of conditions often operating in the shadows, can significantly impact your overall well-being. Using the definition of metabolic syndrome from the International Diabetes Federation (IDF) and the National Cholesterol Education Program, the prevalence of metabolic syndrome is estimated at more than 30 percent in the United States.
What is Metabolic Syndrome?
The syndrome is a multifaceted health condition that quietly lurks in many lives, often overshadowed by more apparent health concerns. Its insidious nature can lead to severe consequences, particularly its close association with diabetes.
What is the Close Connection to Diabetes?
Metabolic syndrome and diabetes are closely interconnected, sharing common underlying factors that contribute to their development. The key components of metabolic syndrome include abdominal obesity, high blood pressure, elevated blood sugar levels, high triglycerides, and low HDL cholesterol.
Insulin Resistance: A central feature linking metabolic syndrome and diabetes is insulin resistance. Insulin is a hormone that helps cells absorb glucose from the bloodstream for energy. In individuals with metabolic syndrome, cells become resistant to the effects of insulin, leading to elevated blood sugar levels. Persistent insulin resistance is a primary factor in the progression from metabolic syndrome to type-2 diabetes.
Abdominal Obesity: Metabolic syndrome often involves the accumulation of visceral fat, particularly around the abdomen. This type of fat is metabolically active and releases substances that contribute to insulin resistance. The excess fat in the abdominal region is associated with an increased risk of developing both metabolic syndrome and diabetes.
Abnormal Cholesterol: Metabolic syndrome is characterized by abnormal lipid profiles, including elevated triglycerides and reduced levels of HDL cholesterol. These lipid abnormalities are associated with insulin resistance and are common in individuals with diabetes. This connection contributes to the progression of metabolic syndrome to diabetes.
Inflammation: Both metabolic syndrome and diabetes involve chronic low-grade inflammation in the body. Inflammation can impair insulin signaling and contribute to insulin resistance. Inflammatory markers such as C-reactive protein (CRP) — a protein made by the liver. The level of CRP increases when there’s inflammation in the body and it is often elevated in individuals with metabolic syndrome and diabetes.
Hypertension: High blood pressure is another component of metabolic syndrome. Hypertension and insulin resistance are interconnected, with one condition often exacerbating the other. Chronic elevation of blood pressure can contribute to the development and progression of diabetes by affecting the cardiovascular system and impairing insulin sensitivity.
Early intervention and a holistic approach are essential to break the link between these conditions and reduce the risk of complications.
The Functional Medicine Approach to Metabolic Syndrome
The functional medicine approach adopts a holistic and personalized approach to address the root causes of the condition. Rather than solely focusing on symptom management, the functional medicine practitioner delves into your unique genetic, environmental, and lifestyle factors to develop a comprehensive, personalized plan.
The first step is to conduct a thorough assessment of your medical history, family history, and lifestyle choices. Understanding the intricate interplay of genetics and environment is crucial in tailoring an individualized plan. Your exercise routine, stress levels, and sleep patterns would be scrutinized to identify potential triggers and contributors to the development of diabetes.
Nutritional therapy would be a cornerstone of your wellness plan. Your dietary habits, food allergies, or sensitivities are a major factor. A functional medicine doctor would work closely with you to create a personalized diet that aims to regulate blood sugar levels, manage weight, and optimize overall health. Emphasizing whole, nutrient-dense foods while minimizing processed sugars and refined carbohydrates would be a fundamental aspect of the dietary recommendations.
Supplementation with vitamins and minerals that play a role in blood sugar regulation may be suggested, based on individual needs. Monitoring progress through regular follow-ups and adjusting the treatment plan accordingly ensures ongoing support and optimization of your health.
By addressing the underlying factors contributing to diabetes within the framework of functional medicine, the practitioner aims to empower you so that you can manage your condition effectively while promoting long-term health and wellness.
“My diabetes doctor told me I would need to take pills for the rest of my life,” said Richard Baird. “I was looking for a different approach. I discovered Angel Longevity Medical Center and I was very impressed. I have been a diabetic for 15 years and this program has made me feel wonderful!”
Watch the testimonial here
By understanding metabolic syndrome, recognizing its components, and embracing a preventive lifestyle, it is possible to take charge of your future well-being. Empowered with this knowledge, you can make informed decisions, break free from the silent threat of metabolic syndrome, and pave the way for a life less susceptible to the clutches of diabetes.
If you have the markers for metabolic syndrome, or already have diabetes, call Dr. Anju for an appointment. Find out if you qualify to become a patient at Angel Longevity Medical Center.